|
Drugs: education, prevention and policy, Vol.
6, 2, 1999 BOBBY P. SMYTH,1
JULIE McMAHON,2 JOHN J. O'CONNOR3 & JIM
RYAN4
1AIDS/Drugs Service, Eastern Health Board, Cherry
Orchard Hospital, Dublin 10, Republic of Ireland; 2James
Connoly Memorial Hospital, Dublin 15, Republic of Ireland; 3Drug
Treatment Centre, McCarthy Centre, Pearse Street, Dublin 2, Republic
of Ireland; 4122 Raheny Road, Dublin 5, Republic of Ireland.
ABSTRACT Hepatitis C (HCV) is very prevalent among injecting drug
users (IDU). Control of this infection poses a major challenge to
harm reduction services. Education of all IDU regarding HCV constitutes
part of the harm reduction programme. We sought to assess understanding
of HCV among IDU attending an addiction treatment clinic and to
identify whether or not those with increased contact with health
professionals demonstrated better understanding. A total of 105
IDU were interviewed to assess their knowledge regarding modes of
transmission and chronicity of HCV infection. They had first infected
an average of 10.0 years previously. Interviewees were more successful
at identifying activities which posed no risk of infection. Over
one-third falsely believed that one could contract HCV infection
even when injecting "safely". Understanding of the long-term
nature of HCV infection was also impaired. A group on methadone
maintenance for a median period of 1.4 years failed to demonstrate
significantly better knowledge than those attending for a 21-day
detoxification. Those in frequent contact with a GP performed less
well than those without such contact. Understanding of HCV among
IDU is inadequate and must improve if primary prevention efforts
are to succeed. We question the value of didactic approaches to
educating IDU and call for a more experiential teaching style which
may be more successful at countering prevalent misconceptions.
World-wide, infection with hepatitis C (HCV) is
common among injecting drug users (IDU) (MacDonald et al., 1996;
Thomas et al., 1995; Wodak & Crofts, 1996). Although UK IDU
have demonstrated a reduction in risk behaviour (Griffin et al.,
1993; Stimson & Hunter, 1996), the prevalence of this infection
remains high in injectors who commenced injecting in the current
era of harm reduction (Smyth et al., 1998). Some commentators have
become quite skeptical about the prospect of reducing rates of HCV
among IDU (Wodak & Crofts, 1996). Internationally, harm reduction
efforts include the provision of sterile injecting equipment and
treatment with methadone. Education regarding safe injecting and
the dangers of unsafe injecting such as HIV and HCV, is another
crucial component and occurs in treatment settings and through community
outreach. All of these approaches are currently in existence in
Dublin. At this point in time there has been no public health awareness
campaign targeting hepatitis C. Therefore, IDU in Dublin are likely
to have acquired information about hepatitis C from one of two main
sources, health professionals and via peers (Barendregt & Trautmann,
1996; Wolitski et al., 1996). Health professionals include general
practitioners and staff working in specialist addiction treatment
centers. The effectiveness of health professionals' attempts to
educate IDU regarding HCV has not previously been assessed. If inadequate,
it may account in part for the ongoing high incidence of HCV
HCV is though to be spread very readily
via sharing needles and syringes. Sexual transmission and vertical
transmission can also occur, although the level of risk associated
with each of these circumstances is less. Now that blood products
are screened for HCV, the risk of infection via blood transfusion
is very much reduced, but is not zero. Up to 90% of infected persons
are thought to carry the virus indefinitely (Cramp & Williams,
1997; Gully & Tepper, 1997).
Two Australian studies have found knowledge of hepatitis C to be
lacking among certain treatment risk groups (prison inmates and
high risk drug users), although the populations studied were not
confined to IDU (Butler et al., 1997; Carruthers & Loxley, 1995).
We sought to measure IDU's level of knowledge regarding HCV in the
setting of an addiction treatment clinic and to identify factors
influencing this knowledge. We anticipated that those with increased
contact with medical services would demonstrate better understanding,
i.e. a 'dose-response' type effect. Also, for those of unknown HCV
status, we wished to assess their current perceived level of risk
of HCV infection.
All patients had a history of injecting
drug use and a diagnosis of opiate dependance. A researcher (JM),
who was independent of treatment services, interviewed patients
over a 5-week period during August and September 1997. The patient
groups eligible for inclusion were (i) those who commenced a 21-day
methadone detoxification during the study period and (ii) those
who attending the clinic daily or on alternate days for methadone
maintenance at the outset of the study. Patients were asked to consent
to a confidential, structured interview lasting 30 min approximately.
Due to time constraints, the researcher could not meet all 139 eligible
patients and consequently 30 (22%) were not asked to participate.
Four of those who were asked to consent to interview refused. The
overall participation rate was 75.5%. Those not interviewed did
not significantly differ in terms of sex ratio or age. Data were
collected on socio-demographics, drug use history, current treatment
and contact with GP.
As no standardized instrument exists for assessing patients' knowledge
regarding HCV, we developed our own series of questions. A scoring
system was also agreed among the research team after consultation
with experts in the area of HCV. We chose to focus on two aspects
of HCV. These were (i) routes of transmission and (ii) chronicity
of infection. Regarding routes of infection, interviewees were initially
asked to identify al routes of transmission which they believed
could lead to HCV infection without prompting. They were then presented
with a list of seven possible modes of spread of hepatitis C and
asked to identify those which they thought were true, false or about
which they were unsure. In order to calculate an overall 'knowledge
score' for each interviewee, the following scoring system was employed.
Correct responses were scored 'plus one', incorrect responses scored
'minus one' and 'don't knows' scored zero. We believed it to be
appropriate to use a 'negative marking system' as a false belief
was considered more hazardous in terms of the individual contracting
and spreading HCV infection, than an acknowledgement of being unsure
regarding a given mode of possible transmission. The two questions
on chronicity of infection followed a multiple choice format, interviewees
being presented with a list of possible answers. Correct responses
to each scored two points, nearly correct responses scored one point
and incorrect responses and 'don't knows' scored zero. The maximum
possible 'knowledge score' was 11. For all questions, interviewees
were asked not to guess Medical terms such as 'vertical' were not
used during questioning with simple lay terminology being substituted.
Seventy-three (70%) of the 105 patients were male.
The median age of the group was 29 years (range 16-48). The median
period since first injecting was 8 years (range 0.2-30years). Forty-three
patients (41%) were on the detoxification programme and 62 (59%)
were on maintenance. Those on maintenance had been attending for
a median period of 1.4 years (range 0.1-20 years). Overall 84 (80%)
reported previously having had a test for hepatitis C, and 75 (89%)
of these indicated that the result was positive.
In all, 77 (73%) indicated that they were registered with a GP.
Of this group, 70 (91%) reported that their GP was aware of their
drug use and 47 (61%) had seen their GP six or more times over the
preceding 12 months.
All participants had heard of hepatitis C. Table 1 indicates that
the cast majority (90%) spontaneously identified sharing injecting
equipment as being a risk activity for transmission of hepatitis
C. Sexual intercourse and receiving a blood transfusion were the
next two most frequently reported potential modes of transmission.
Table 2 indicates responses when interviews were asked directly
about specific activities. In all, 77 (73%) recognized all four
of the risk activities (i.e. sharing injecting equipment, sex, transfusion
and vertical). The proportions responding correctly dropped when
asked about activities with no recognized risk with only 46 (44%)
recognizing all three 'safe' activities (i.e. injecting without
sharing, smoking heroin and kissing). On the issue of chronicity
of infection, only 46 (44%) answered both questions correctly.
Over one-third incorrectly believed that on could contract HCV while
injecting safely, i.e. when no sharing of any injecting equipment
or associated paraphernalia occurred (Table 2). Those who believed
this were subsequently questioned about how this might occur to
ensure that they were not misunderstanding the question. Theories
about this mode of transmission varied but included; 'if your own
blood is exposed to the air when you draw back, you can get it',
'its on your skin and once you push the needle through, you get
it' or 'it can just be in the gear (Heroin)'.
Regarding the overall 'knowledge score', these ranged from minus
1 to 11 (mean 7.60, median 8). Only 18 (17%) of interviewees responded
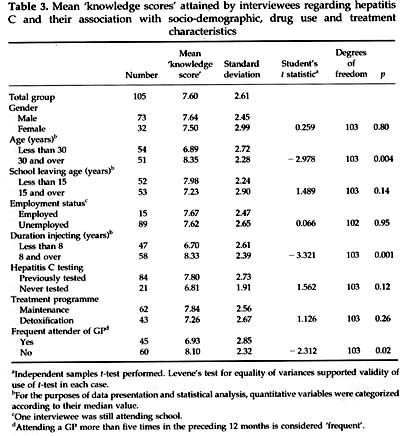
correctly to all questions. Table 3 shows the relationship between
the mean 'knowledge score'
| Table 1
The proportion of interviewees reporting various methods of
transmission of hepatitis C in response to an open-ended question,
without prompting |
| |
Total
(n=105) |
Males
(n=73) |
Females
(n=32) |
Significance
Testa |
|
|
|
|
|
|
|
|
|
Number |
% |
Number |
% |
Number |
% |
% |
| 95 |
90 |
67 |
92 |
28 |
88 |
0.49 |
Sexual
intercourse |
49 |
47 |
35 |
48 |
14 |
44 |
0.69 |
Receiving
a blood transfusion |
20 |
19 |
15 |
20 |
5 |
16 |
0.55 |
Injecting
without ever sharing injecting equipment |
8 |
8 |
7 |
10 |
1 |
3 |
0.43 |
| Household
spread (toothbrushes, etc.) |
8 |
8 |
7 |
10 |
1 |
3 |
0.43 |
Kissing |
1 |
1 |
1 |
1 |
0 |
0 |
1.0 |
Vertical |
0 |
0 |
0 |
0 |
0 |
0 |
1.0 |
|
|
|
|
|
|
|
|
and various independent variables. Older age and
longer history of injecting were each associated with significantly
better scores (p<0.01). (It must be noted that the groupings
for age tending also to have longer injecting histories (chisquared
= 33.9, p<0.001). Those in frequent contact with a GP did significantly
worse than those without such contact (p=0.02). Neither younger
interviewees nor those with shorter injecting histories were over-represented
in the group with frequent GP contact (data not shown, chi squared
test, p=0.73 and 0.74, respectively). Gender, remaining longer in
education, employment status, having previously tested for HCV and
being on the maintenance programme were not significantly associated
with better scores.
Of the 21 never previously tested for HCV, only five thought it
likely or very likely that they were currently infected.
This study has some limitations. Firstly, only
75.5% of the available study population were interviewed due to
time constraints imposed on the number of weeks during which the
interviewer could attend the clinic. However, we believe that it
is unlikely that any sampling bias was inherent in this process.
The study population is modest in size and hence limited the power
to detect possible independent variables which exert a minor effect
on knowledge enhancement. Also in this study population, the mean
age is greater and mean length of injecting history longer than
the corresponding figures from the national statistics on attendances
for treatment of drug misuse (Moran et al., 1997). This suggests
that the level of knowledge demonstrated in this study is greater
than one would expect of the typical IDU attending for treatment
in Dublin. Also, we did not attempt to assess understanding of the
various degrees.
|
|
|
|
|
|
|
|
| Table 2
Beliefs held by interviewees regarding specific potential
modes of transmission of hepatitis C and responses to questions
on chronicity of infection |
|
|
|
|
|
|
|
|
|
|
Correctly
responding |
Incorrectly responding |
Unsure |
|
|
|
|
|
|
|
|
| |
Number |
% |
Number |
% |
Number |
% |
|
|
|
|
|
|
|
|
| Identification of activities that pose some
level of risk |
|
|
|
|
|
|
|
|
| Sharing injecting equipment |
104 |
99 |
0 |
0 |
1 |
1 |
| Sexual intercourse |
96 |
91 |
4 |
4 |
5 |
5 |
| Receiving a blood transfusion in the past |
96 |
91 |
4 |
4 |
5 |
5 |
| Vertical |
90 |
86 |
7 |
7 |
8 |
7 |
| All four identified as posing some level of
risk |
77 |
73 |
|
|
|
|
|
|
|
|
|
|
|
|
| Identification of activities that pose no recognized
risk |
|
|
|
|
|
|
|
|
| Injecting without ever sharing injecting equipment |
59 |
56 |
39 |
37 |
7 |
7 |
| Only ever smoking heroin |
84 |
80 |
16 |
15 |
5 |
5 |
| Kissing |
87 |
83 |
11 |
10 |
7 |
7 |
| All three identified as posing no risk |
46 |
44 |
|
|
|
|
|
|
|
|
|
|
|
|
| 'How long does hepatitis C usually stay in the
body when infected?' |
|
|
|
|
|
|
|
|
| Days to months |
|
|
2 |
2 |
|
|
| Many years |
6 |
6 |
|
|
|
|
| Lifetime |
74 |
70 |
|
|
|
|
| Don't know |
|
|
|
|
23 |
22 |
|
|
|
|
|
|
|
|
| How many people with hepatitis C Will have infection
for years? |
|
|
|
|
|
|
|
|
| 10% or less |
|
|
10 |
9 |
|
|
| About 1 in 3 |
1 |
1 |
|
|
|
|
| More than half (more than 50%) |
51 |
49 |
|
|
|
|
| Don't know |
|
|
|
|
43 |
41 |
| Both questions on 'chronicity answered correctly |
46 |
44 |
|
|
|
|
|
|
|
|
|
|
|
|
of risk associated with activities, sharing of injecting equipment
obviously carrying with it a much greater level of risk than sexual
intercourse, for example. The use of face-to-face interviews, which
were conducted by a member of the research team with clinical training,
ensuring that misunderstanding of questions by interviewees was kept
to a minimum.
Encouraging findings included the fact that all had heard of HCV and
knowledge of the risk activities which may lead to its transmission
were satisfactory. This was not the case in the two Australian populations
previously studied and may indicate the beneficial impact of contact
with treatment services. However, greater confusion was demonstrated
when it came to
 independent samples t-test performed. Levene`s
test for equality of variances supported validity of use of t-test
in each case. bFor the purposes of data presentation
and statistical analysis, quantitative variables were categorized
according to their median value. cOne interviewee was
still attending school. dAttending a GP more than five
times in the preceding 12 months is considered `frequent`.
fying those activities which posed no risk of
HCV. We are concerned at the finding that substantial minorities
believe that there is risk of exposure even when not sharing any
injecting paraphernalia and when only smoking heroin. Perceived
personal vulnerability to infections such as HCV is likely to be
a factor in leading individuals to avoid practising unsafe injecting
(Carruthers & Loxley, 1995). If this vulnerability is diminished
by a false belief that one may already have been exposed to HCV
when injecting safely or when smoking, the preparedness to share
injecting equipment may well increase. Hence such misconceptions
may facilitate spread of HCV and HIV. IDUs' underestimation of their
level of risk of exposure to HCV was demonstrated and this is a
frequent finding in studies of this nature (Carruthers & Loxley,
1995).
Those participants who were on the maintenance programme had been
attending for a median period of over 500 days. The maximum attendance
period for those on the detoxification programme prior to interview
was 25 days, but was much less in most cases (exact period of attendance
not recorded for the detoxification group). The fact that those
on the maintenance programme did not know significantly more about
HCV suggests that prolonged and ongoing contact with a treatment
center is not significantly better in terms of knowledge acquisition
than a brief contact. The finding that those in regular contact
with a GP performed less well than those without such contact was
surprising. We were unable to identify any confounding variable
which could explain this observation. Overall, we found no evidence
that health professional contact and knowledge acquisition demonstrated
a positive 'dose-response effect'.
In this highly treated population of IDU, many still demonstrated
prominent misconceptions about the ease of transmission and natural
history of HCV infection. Simply increased contact with services
has not been shown here to lead to any significant gain in understanding.
Hence one must conclude that current education approaches in specialist
treatment centers and by GPs have deficits. There may be inadequate
understanding of HCV among drug service workers and this could be
usefully examined in further studies. Alternatively, rather than
a lack of knowledge, there may be inadequacies in the way in which
information is provided to IDU. Stiernborg et al. (1996) evaluated
HIV educational approaches and demonstrated that a didactic teaching
style is less effective than an experiential style. It may well
be the case that as health professionals, we are more inclined to
give facts to patients about what we know to be the risk activities,
rather than explore with them what they perceive as risk behaviour.
When adopting the latter approach, their misconceptions are more
likely to emerge and thereby provide the clinician with the opportunity
to correct and educate. This approach is amenable to group work
(Stiernborg et al., 1996). If misconceptions are not corrected on
contact with health professionals, then the potentially useful peer
network will only serve to perpetuate misinformation (Barendregt
& Trautmann, 1996).
We accept that even if all IDU were fully informed, injecting risk
behaviour would not cease. However, we firmly believe that extensive
syringe exchange programmes, without co-existing focused education
approaches, will fall far short of their potential impact (Smith,
1987; Strathdee et al., 1997). There is a need for thoughtful education
initiatives, which take into account the various myths and misconceptions
which are prevalent in each given area world-wide. This means moving
away from the typical didactic model of fact provision.
The authors wish to acknowledge the co-operation of the staff of
McCarthy Centre in facilitating this study. We also wish to express
our gratitude to Dr Eamon Keenan for his advice and criticism in
the preparation of this manuscript and to Dr Saeed Al-Bloushi and
Dr Shay Keating for their advice regarding the scoring system used
in this study. We are grateful for the generous funding received
from the AIDS/Drugs Service of the Eastern Health Board, Dublin
and from the Charitable Trust of The Charitable Infirmary, Dublin.
BARENDREGT, C.& TRAUMANN, F. (1996). With a Little Help from
my Friends: a survey on non-intentional peer influences among drug
users. Utrecht, Netherlands: National Institute for Alcohol and
Drugs.
BUTLER, T.G., DOLAN, K.A., FERSON, M.J., McGUINESS, L.M. et al.
(1997) Hepatits B and C in New South Wales prisons: prevalence and
risk factors. Medical Journal of Australia, 166pp. 127-30.
CARRUTHERS, S. & LOXLEY, W. (1995). Hepatitis C and young drug
users: are they about to join the epidemic? Australian Journal of
Public Health, 19, pp. 421-24.
CRAMP, M.E. & WILLIAMS, R. (1997). Hepatitis in alcohol and
drug misusers: practical issues. Addiction Biology, 2, pp. 411-19.
GRIFFIN, S., PETERS, A. & REID, M. (1993). Drug misusers in
Lothian: changes in injecting habits 1988-90. BMJ, 306, p. 693.
GULLY, P.R. & TEPPER, M.L, (1997) Hepatitis C. Canadian Medical
Association Journal, 156, pp. 1427-28.
MACDONALD, M. CROFTS, N. & KALDOR, J. (1996). Transmission of
hepatitis C virus: rates, routes and cofactors. Epidemiologic Reviews,
18, pp. 137-48.
MORAN, R., O`BRIEN, M., & DUFF, P., (1997). Treated Drug Misuse
in Ireland: National Report 1996. Dublin: Health Research Board
SMITH, D.E. (1987). The role of substance abuse professionals in
the AIDS epidemic. Advances in Alcohol & Substance Abuse, 7(20),
pp. 175-95.
SMYTH, B., KEENAN, E. & O`CONNOR, J. (1998). Bloodborne viral
infection in Irish injecting drug users. Addiction, 93, pp 1649-56.
STIERNBORG, M., ZALDIVAR, S.B., & SANTIAGO, E.G. (1996). Effect
of didactic teaching and experiential learning on nursing students
AIDS related knowledge and attitudes. AIDS Care, 8, pp. 601-8.
STIMSON, G.V. & HUNTER, G. (1996). Interventions with drug injectors
in the UK: trends in risk behaviour and HIV prevalence. International
Journal of STD and AIDS, 7, pp.52-56.
STRATHDEE, S.A. PATRICK, D.M. CURRIE, S.L., CORNELISSE, P.G. et
al. (1997). Needle exchange is not enough: lessons from the Vancouver
injecting drug use study. AIDS, 11(8), pp. 59-65.
THOMAS, D.L., VLAHOV, D., SOLOMON, P.H., COHN, S. et al. (1995).
Correlates of hepatitis C infections among injection drug users.
Medicine, 74, pp. 212-20.
WODAK, A. & CROFTS, N. (1996). Once more unto the breach: controlling
hepatitis C in injecting drug users, Addiction, 91, pp.181-84.
WOLITSKI, R.J., FISHNEIN, M. JOHNSON, W.D., SCHNELL, D.J. et al.
(1996). Sources of HIV information among injecting drug users: association
with gender, ethnicity, and risk behaviour. AIDS Care, 8, pp. 541-55.
|

